Table of Contents
Mesh Repair

Mesh repair is a surgical procedure commonly used to treat various medical conditions, particularly hernias. It involves the placement of a synthetic mesh material to reinforce weakened or damaged tissue, providing support and preventing recurrence. In this blog post, we’ll delve into the intricacies of mesh repair, covering its purpose, procedure, potential risks, and recovery process.
Understanding Mesh Repair:
Mesh repair is primarily employed in the treatment of hernias, which occur when an organ or fatty tissue protrudes through a weak spot in the surrounding muscle or connective tissue. Hernias can develop in different areas of the body, including the abdomen, groin, and even the diaphragm.
The primary goal of mesh repair is to strengthen the weakened area and reduce the risk of recurrence. The synthetic mesh used in the procedure serves as a scaffold, promoting tissue growth and providing long-term reinforcement.
Herniectomy
Herniectomy, also known as hernia repair surgery, is a common procedure performed to correct hernias, which occur when an organ or fatty tissue protrudes through a weak spot in the surrounding muscle or connective tissue
Understanding Herniectomy:
Herniectomy is a surgical procedure aimed at repairing hernias by returning the displaced tissue to its proper position and reinforcing the weakened area to prevent recurrence. Hernias can develop in various parts of the body, including the abdomen, groin, and diaphragm, and they can cause discomfort, pain, and other complications if left untreated.
The primary objectives of herniectomy are to relieve symptoms, prevent complications such as incarceration or strangulation, and restore normal function and appearance to the affected area. The procedure can be performed using different surgical techniques, including open surgery or minimally invasive approaches such as laparoscopy.
Mesh repair/ Herniectomy – Procedure Overview:
The herniectomy/mesh repair procedure typically involves the following steps:
- Anesthesia: The patient is administered either local or general anesthesia to ensure comfort during the surgery.
- Incision: The surgeon makes an incision near the site of the hernia, providing access to the affected area.
- Hernia Reduction: If necessary, the protruding tissue is gently pushed back into place.
- Repair: The surgeon reinforces the weakened area using various techniques, such as suturing the muscle or tissue layers together or using synthetic mesh to provide additional support.
- Closure: The incision is closed with sutures or surgical staples.
The specific approach and techniques used may vary depending on factors such as the size and location of the hernia, the patient’s medical history, and the surgeon’s preference.
Mesh repair/ Herniectomy – Potential Risks:
While herniectomy/mesh repair is generally considered safe and effective, like any surgical procedure, it carries certain risks and potential complications, including:
- Infection at the surgical site
- Bleeding
- Damage to nearby structures, such as blood vessels or nerves
- Recurrence of the hernia
- Chronic pain or discomfort
- Adverse reactions to anesthesia
It’s essential for patients to discuss these potential risks with their healthcare provider and weigh them against the benefits of the procedure.
Mesh repair/ Herniectomy – Recovery Process:
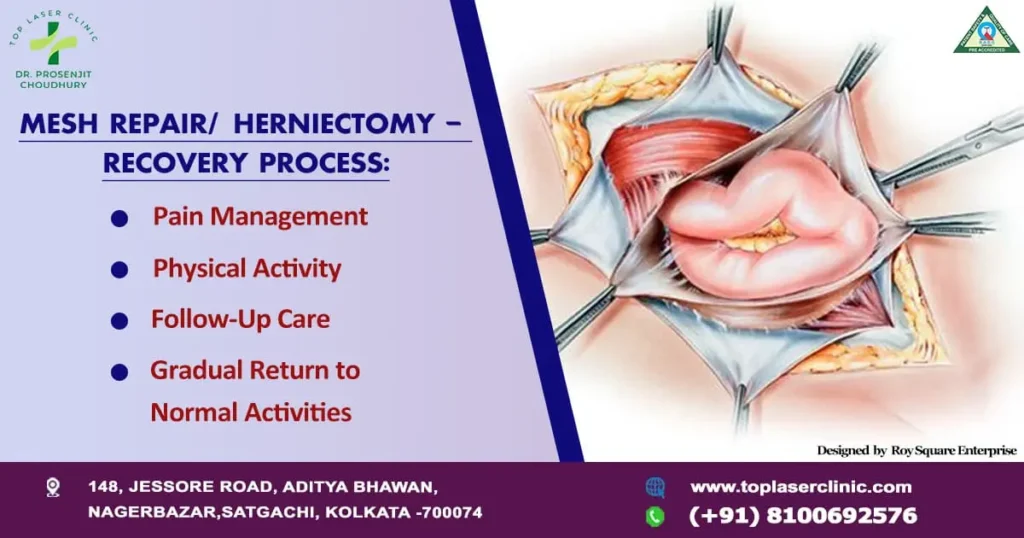
Recovery from herniectomy surgery varies depending on factors such as the type of hernia, the surgical approach used, and individual healing capabilities. However, some general guidelines apply:
- Pain Management: Pain and discomfort following surgery are common and can be managed with prescribed medications.
- Physical Activity: Patients are typically advised to avoid strenuous activities and heavy lifting for several weeks to allow adequate healing.
- Follow-Up Care: Regular follow-up appointments with the surgeon are essential to monitor healing progress and address any concerns.
- Gradual Return to Normal Activities: Patients can gradually resume normal activities as directed by their healthcare provider.
It’s crucial for patients to adhere to post-operative instructions and attend all follow-up appointments to ensure a smooth recovery and minimize the risk of complications.
Herniectomy is a valuable surgical procedure used to repair hernias and alleviate associated symptoms and complications. Even if there are many advantages, patients must fully comprehend the operation, any hazards, and the recuperation period. Patients can minimize the risk of problems and achieve the best possible results by carefully collaborating with their healthcare providers and adhering to post-operative instructions.
Meshoma
Meshoma, also known as mesh-related complications, refers to a range of issues that can arise following surgical procedures where mesh implants are used. Meshoma can encompass various complications, including inflammation, infection, mesh migration, and chronic pain. These complications can occur after hernia repair surgeries, pelvic organ prolapse repair, or other procedures where synthetic mesh materials are implanted to reinforce weakened or damaged tissue.
Understanding Meshoma:
Meshoma can manifest in different ways, depending on the type of complication and its severity. Some common types of meshoma include:
- Inflammation: Inflammatory reactions to the mesh material can lead to swelling, redness, and discomfort at the surgical site. Severe inflammation may require medical intervention to alleviate symptoms and prevent further complications.
- Infection: The presence of foreign material like mesh increases the risk of infection. Symptoms of infection may include fever, drainage from the surgical site, and increased pain. In severe cases, surgical intervention or antibiotic therapy may be necessary to treat the infection.
- Mesh Migration: Mesh migration occurs when the implanted mesh shifts from its original position, potentially causing pain, discomfort, and complications such as bowel obstruction or perforation. Surgical removal of the migrated mesh may be required to resolve these issues.
- Chronic Pain: Some patients may experience persistent or recurrent pain following mesh implantation. This can be due to nerve damage, mesh contraction, or other factors. Management of chronic pain may involve medication, physical therapy, or additional surgical procedures.
- Mesh Contraction: Over time, some types of mesh implants can contract or shrink, leading to complications such as mesh folding, distortion of surrounding tissue, and recurrence of hernias or prolapse. Revision surgery may be necessary to address these issues.
Management and Treatment:

The management of meshoma depends on the specific complications involved and their impact on the patient’s health and well-being. Treatment options may include:
- Conservative Management: In mild cases of mesh-related complications, conservative measures such as pain medication, anti-inflammatory drugs, and physical therapy may be sufficient to alleviate symptoms.
- Surgical Intervention: In more severe cases, surgical removal of the mesh implant or revision surgery may be necessary to address complications such as infection, mesh migration, or chronic pain. Surgeons may opt for open surgery or minimally invasive techniques, depending on the individual circumstances.
- Multidisciplinary Care: Managing meshoma often requires a multidisciplinary approach involving surgeons, pain management specialists, infectious disease specialists, and other healthcare providers. Collaboration among these professionals ensures comprehensive care tailored to the patient’s needs.
Prevention:
Preventing meshoma involves careful patient selection, meticulous surgical technique, and appropriate mesh selection. Surgeons should thoroughly assess patients for risk factors such as previous mesh-related complications, allergies, and comorbidities before recommending mesh implantation. Additionally, proper surgical placement and adherence to established guidelines can help minimize the risk of complications.
Meshoma represents a spectrum of complications that can occur following surgical procedures involving mesh implants. While these complications can pose challenges for patients and healthcare providers, prompt recognition, appropriate management, and multidisciplinary care can help mitigate the impact of mesh-related issues and improve patient outcomes. By prioritizing patient safety and adherence to best practices, surgeons can minimize the risk of meshoma and optimize the benefits of mesh implantation in appropriate cases.
Hernia