Table of Contents
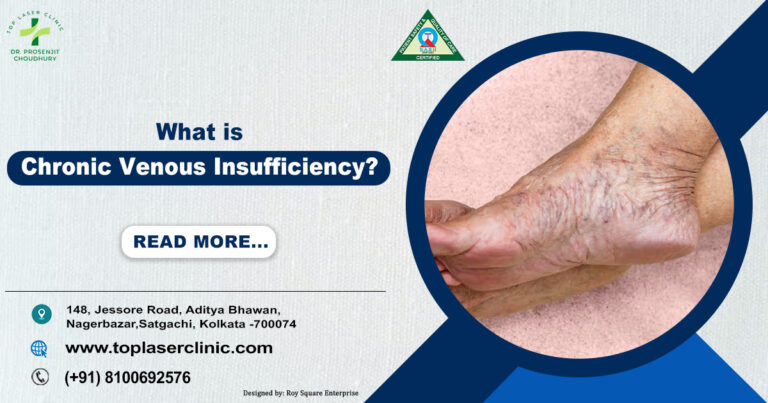
Chronic Venous Insufficiency (CVI) is a widespread but frequently neglected condition that impacts millions of individuals globally. It occurs when the veins in your legs fail to efficiently return blood to your heart. CVI results in blood accumulation in the veins of the legs, causing increased pressure within those veins, leading to a range of uncomfortable and sometimes severe symptoms. Chronic Venous Insufficiency (CVI) can occur as a result of damage to any of the veins in your legs. These veins include:
– Deep veins: Larger veins located deep within the body, running through muscle tissue.
– Superficial veins: Veins situated closer to the surface of the skin.
– Perforating veins: Veins that link the deep and superficial veins together.
CVI may start mildly but over time, it may lead to serious complications. If left untreated, CVI can significantly impact your quality of life.
What is Chronic Venous Insufficiency?
Chronic Venous Insufficiency (CVI) is a medical condition in which the veins in the legs have difficulty returning blood to the heart. Normally, tiny valves in your veins ensure that blood flows upward, against gravity. However, when these valves become weak or damaged, blood can pool in your legs, leading to swelling, pain, and other complications. CVI is often associated with varicose veins, but it’s more than just a cosmetic issue—it’s a medical condition that requires attention.
Causes of Chronic Venous Insufficiency
Understanding the cause ofchronic venous insufficiency is crucial for prevention and treatment. Here are the primary factors that contribute to CVI:
1. Damaged Vein Valves:
Damaged or weakened vein valves are the most common cause of chronic venous insufficiency (CVI). These tiny, one-way valves in your veins ensure blood flows upward to the heart. When they fail, blood leaks backward and pools in the veins, leading to swelling, pain, and varicose veins.
- Why Do Valves Fail?
– Aging: Valves lose elasticity over time.
– Prolonged Standing/Sitting: Increases pressure on leg veins.
– Hormonal Changes: Pregnancy or menopause can weaken valves.
– Blood Clots: DVT can scar and damage valves.
– Genetics: Family history plays a role.
- The Domino Effect
Damaged valves cause blood to pool, stretching veins and worsening symptoms like swelling, skin changes, and ulcers over time.
- Prevention Tips
– Stay active with walking or swimming.
– Take breaks from sitting or standing.
– Elevate your legs daily.
– Wear compression stockings for support.
By understanding and addressing valve damage, you can take proactive steps to protect your vein health and prevent CVI.
2. Deep Vein Thrombosis (DVT):
A history of Deep Vein Thrombosis (DVT)—blood clots in the deep veins—can damage vein valves, leading to chronic venous insufficiency (CVI). When a clot forms, it can scar the veins and disrupt valve function, causing blood to pool and increasing pressure in the veins.
- Why DVT Leads to CVI
– Blood clots damage vein walls and valves.
– Scarring from DVT prevents proper blood flow.
– Increased pressure in veins worsens over time.
- Prevention Tips
– Stay active to improve circulation.
– Avoid prolonged sitting or standing.
– Seek treatment for DVT promptly to reduce long-term damage.
Addressing DVT early can help protect your veins and prevent CVI.
3. Obesity:
Carrying excess weight puts added pressure on your veins, increasing the risk of valve damage and CVI . The extra weight strains the veins in your legs, making it harder for them to pump blood back to the heart.
- Why Weight Matters
– Increased pressure weakens vein valves.
– Poor circulation worsens blood pooling.
– Higher risk of swelling, varicose veins, and skin changes.
- Prevention Tips
– Balance a healthy weight through diet and exercise.
– Stay active to improve blood flow.
– Wear compression stockings for added support.
4. Pregnancy:
It can strain your veins due to hormonal changes and increased blood volume, raising the risk of CVI . The growing uterus also puts pressure on the veins in your pelvis, making it harder for blood to flow from your legs back to your heart.
- Why Pregnancy Affects Veins
– Hormones relax vein walls, weakening valves.
– Increased blood volume adds pressure to veins.
– The uterus compresses pelvic veins, slowing circulation.
- Prevention Tips
– Stay gently active with safe and light exercises like walking or mild swimming.
– Elevate your legs to reduce swelling.
– Wear maternity compression stockings for support.
While these changes are often temporary, taking steps to support your veins during pregnancy can help prevent CVI.
5. Sedentary Lifestyle:
A sedentary lifestyle weakens the muscles that help pump blood, increasing the risk of CVI. Inactivity slows blood flow, causing pooling and pressure in the veins.
- Prevention Tips
– Move regularly—take short walks or stretch.
– Exercise daily to boost circulation.
– Wear compression stockings for support.
Stay active to protect your veins and prevent CVI.
6. Genetics:
It can make you more prone to developing CVI . If your parents or siblings have vein problems, you may inherit weaker vein valves or vein walls, increasing your risk.
- Why Genetics Matter
– Weak vein valves or walls can run in families.
– Higher likelihood of blood pooling and valve damage.
– Early awareness is key to prevention.
- Prevention Tips
– Stay active to support vein health.
– Wear compression stockings if at risk.
– Monitor for symptoms like swelling or varicose veins.
While you can’t change your genes, proactive steps can help manage your risk of CVI.
Symptoms of Chronic Venous Insufficiency
Recognizing the symptoms of chronic venous insufficiency Early can help you seek timely treatment. Common symptoms include:

1. Swelling in the lower limbs (edema: Fluid buildup in legs and ankles due to poor blood flow, often worsening after standing or sitting for long periods.
2. Aching or cramping in the legs: Dull pain or sudden cramps caused by blood pooling and increased pressure in the veins.
3. Heaviness or fatigue in the legs: A constant tired or heavy feeling, especially after activity, due to inefficient circulation.
4. Itchy or irritated skin: Dry, itchy skin around the ankles or lower legs caused by poor blood flow and fluid buildup.
5. Varicose veins:Swollen, twisted veins visible under the skin, resulting from weakened valves and blood pooling.
6. Skin discoloration:Brown or red patches near the ankles caused by blood leaking into surrounding tissues.
7. Ulcers or open sores:Painful, non-healing wounds near the ankles due to severe circulation problems and tissue damage.
If you experience any of these symptoms, it is crucial to seek advice from a healthcare professional for an accurate diagnosis.
Stages of Chronic Venous Insufficiency
CVI progresses through several stages, each with its own set of symptoms and complications. Understanding the stages of chronic venous insufficiency can help you monitor the condition and seek appropriate treatment:
1. Stage 0: No visible signs, but you may experience mild discomfort or fatigue in the legs.
2. Stage 1: Spider veins or reticular veins appear, along with mild swelling.
3. Stage 2: Varicose veins become noticeable, accompanied by swelling and aching.
4. Stage 3: Swelling worsens, and skin changes like discoloration or dryness occur.
5. Stage 4: Skin ulcers develop, indicating advanced CVI.
6. Stage 5 (Healed Venous Ulcer): The ulcer has fully healed, though the risk of recurrence remains if venous issues persist.
7. Stage 6 (Active Venous Ulcer): Open ulcers are present, often causing pain and swelling, requiring proper care for healing.
Early intervention can prevent the condition from progressing to later stages.
Treatment of Chronic Insufficiency
Chronic Venous Insufficiency (CVI) happens when your veins struggle to send blood back to your heart, often causing swelling, pain, and discomfort in your legs. The good news? There are many ways to manage and treat CVI effectively. Let’s understand those:
1. Compression Therapy: Your Legs’ Best Friend
– What it is:Compression stockings are special socks or sleeves that gently squeeze your legs. This pressure helps your veins push blood back up to your heart.
– Why it works:Think of it like giving your veins a little hug to keep things moving smoothly. It’s one of the easiest and most effective ways to reduce swelling and discomfort.
– Pro Tip:Wear them daily, especially if you’re on your feet a lot or sitting for long periods.
2. Lifestyle Changes: Small Steps, Big Results
– Move More: Regular exercise, like walking or swimming, keeps your blood flowing and strengthens your leg muscles.
– Watch Your Weight: Extra weight can put pressure on your veins, so maintaining a healthy weight helps.
– Avoid Sitting or Standing Too Long:Take breaks to stretch or walk around. If you’re stuck at a desk, try flexing your feet or doing leg lifts to keep blood moving.
3. Medications: A Helping Hand from Your Doctor
– What they do: Your doctor might prescribe medicines to reduce swelling, prevent blood clots, or improve vein health.
– Examples:Diuretics (to reduce fluid buildup) or blood thinners (to prevent clots).
– Remember: Always follow your doctor’s advice and never self-medicate.
4. Minimally Invasive Procedures: Quick Fixes for Damaged Veins
– What they are:These are simple procedures that don’t require major surgery. They’re done in a clinic or hospital, and you can usually go home the same day.
– Types:
– Sclerotherapy:A specific solution is introduced into the vein to seal it off.
– Endovenous Laser Treatment (EVLT): A tiny laser is used to seal the damaged vein.
– Radiofrequency Ablation: Heat is used to close the vein.
– Why they’re great: They’re quick, effective, and have minimal downtime.
5. Surgery: For Severe Cases
– When it’s needed: If other treatments don’t work, or if your CVI is very advanced, surgery might be an option.
– Types:
– Vein Stripping: Damaged veins are removed through small cuts.
– Bypass Surgery: A healthy vein is used to reroute blood flow around a blocked vein.
– Recovery:It may take a few weeks to heal, but it can provide long-term relief.
Bonus Tips for Managing CVI:
– Elevate Your Legs:Prop your legs up on a pillow or stool for 15-20 minutes a few times a day. This helps blood flow back to your heart.
– Stay Hydrated: Drinking plenty of water keeps your blood from getting too thick, which makes it easier to circulate.
– Eat a Vein-Healthy Diet:Foods rich in fiber (like fruits, veggies, and whole grains) and low in salt can help reduce swelling and improve circulation.
– Quit Smoking:Smoking damages blood vessels and makes CVI worse. Kicking the habit can improve your vein health.
Best Compression Stocking for Venous Insufficiency
Compression stockings are a cornerstone of CVI treatment. But with so many options available, how do you choose the Best compression stocking for venous insufficiency? Here’s what to look for:
– Graduated Compression:Stockings should provide the most pressure at the ankle and gradually decrease up the leg.
– Proper Fit: Ensure the stockings fit snugly but comfortably. Ill-fitting stockings can worsen symptoms.
– Material:Opt for breathable, moisture-wicking materials to avoid skin irritation.
– Compression Level: Your doctor may recommend mild (15-20 mmHg), moderate (20-30 mmHg), or firm (30-40 mmHg) compression based on your condition.
Popular brands like Medi, Jobst, and Sigvarisare known for their high-quality compression stockings. Always consult your healthcare provider before making a purchase.
Preventing Chronic Venous Insufficiency
While some risk factors like genetics can’t be changed, you can take steps to reduce your risk of developing CVI:

– Stay Active: Regular exercise, especially walking, can improve circulation.
– Elevate Your Legs:Elevating your legs above heart level for 15-20 minutes daily can reduce swelling.
– Avoid Tight Clothing:Tight clothes can restrict blood flow.
– Stay Hydrated:Maintaining adequate hydration promotes healthy blood circulation.
When to See a Doctor
If you experience persistent symptoms of chronic venous insufficiency, such as swelling, pain, or skin changes, it’s important to seek medical advice. Early diagnosis and treatment can prevent complications like ulcers or blood clots.
Call-to-Action
Don’t let chronic venous insufficiency disrupt your life. If you’re experiencing symptoms or have concerns about your vein health, consult a healthcare professional today. Early intervention can make all the difference. For those already diagnosed, consider investing in the best compression stocking for venous insufficiency to manage your symptoms effectively. Your veins will thank you!
Here are some FAQs :
1. What is Chronic Venous Insufficiency (CVI)?
Answer:
Chronic Venous Insufficiency (CVI) is a medical condition in which the veins in the legs have difficulty returning blood to the heart.This happens because the valves in your veins become weak or damaged, causing blood to pool in your legs. It may result in symptoms such as swelling, discomfort, and the development of varicose veins.
2. What is the primary reason behind the development of venous insufficiency?
Answer:
The primary reason for venous insufficiency is the impairment or weakening of vein valves. Other contributing factors include:
– Aging
– Deep Vein Thrombosis (DVT)
– Obesity
– Pregnancy
– Prolonged sitting or standing
– Genetics
3. What are the initial signs of chronic venous insufficiency?
Answer:
The early symptoms of chronic venous insufficiency include:
– Swelling in the legs and ankles
– Aching or cramping in the legs
– Feeling of heaviness or fatigue
– Itchy or irritated skin
– Mild varicose veins
4. How is chronic venous insufficiency diagnosed?
Answer:
CVI is diagnosed through:
– Physical Examination: Checking for swelling, varicose veins, or skin changes.
– Ultrasound: To assess blood flow and valve function.
– Venogram: A special X-ray to visualize vein structure.
5. What are the different stages of chronic venous insufficiency?
Answer:
The stages of chronic venous insufficiency are:
1. Stage 0: No visible signs, mild discomfort.
2. Stage 1: Spider veins, mild swelling.
3. Stage 2: Varicose veins, noticeable swelling.
4. Stage 3: Skin changes like discoloration or dryness.
5. Stage 4: Ulcers or open sores.
6. What is the most effective treatment for chronic venous insufficiency?
Answer:
Some effective treatments for chronic venous insufficiency :
– Compression Stockings: Improve blood flow.
– Lifestyle Changes: Do exercise, weight management, and proper leg elevation.
– Medications: It helps to reduce swelling or prevent clots.
– Minimally Invasive Procedures: Like sclerotherapy or laser treatment.
– Surgery: For severe cases.
7. Are compression stockings effective for CVI?
Answer:
Yes, compression stockings are highly effective for CVI. They:
– Improve blood circulation.
– Reduce swelling and discomfort.
– Prevent complications like ulcers.
Choose the **best compression stocking for venous insufficiency** with the right fit and compression level (as recommended by your doctor).
8. Can chronic venous insufficiency be cured?
Answer:
While CVI cannot be completely cured, it can be effectively managed with:
– Proper treatment (compression therapy, medications, or procedures).
– Lifestyle changes (exercise, healthy diet, and avoiding prolonged sitting/standing).
Timely intervention can stop the condition from getting worse.
9. What happens if chronic venous insufficiency is left untreated?
Answer:
If left untreated, CVI can lead to:
– Severe swelling and pain.
– Skin ulcers (open sores).
– Blood clots (deep vein thrombosis).
– Permanent skin damage or discoloration.
Early medical approach can give you good health back.
10. How can I prevent chronic venous insufficiency?
Answer:
You can prevent CVI by:
– Staying active (walking, swimming, or cycling).
– Maintaining a healthy weight.
– Elevating your legs daily.
– Avoiding tight clothing.
– Wearing compression stockings if you’re at risk.