What Are ZSR Circumcision Procedures?
ZSR circumcision is a modern, minimally invasive circumcision technique performed using a specialized stapler-like device known as the ZSR Stapler. This method ensures a clean cut, minimal bleeding, faster healing, and significantly lower discomfort compared to traditional circumcision methods.
The procedure removes the foreskin using controlled, precise pressure and seals the wound simultaneously using medical-grade staples. As a result, patients experience:
- Shorter procedure time
- Less pain
- Reduced risk of infection
- Better cosmetic results
- A quicker return to daily activities
The ZSR technique is particularly popular among adults and adolescents seeking a safe and advanced circumcision option.
At Top Laser Clinic, Dr. Prosenjit Choudhury, one of the best general surgeons in Kolkata, performs ZSR with outstanding precision, ensuring a comfortable and smooth patient experience.

Who Is an Ideal Candidate for ZSR Circumcision?
ZSR circumcision is a modern, minimally invasive circumcision technique that uses a stapler-based device to remove the foreskin with precision, less pain, and faster healing compared to traditional methods. It has become a popular choice for both adults and adolescents because it is quick, safe, and offers excellent cosmetic results.
But who is the right candidate for ZSR? Here’s a simple breakdown.
You Are an Ideal Candidate for ZSR If You Have:
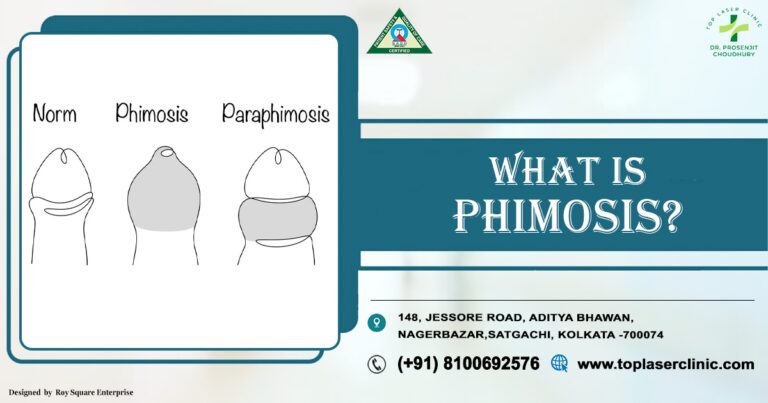
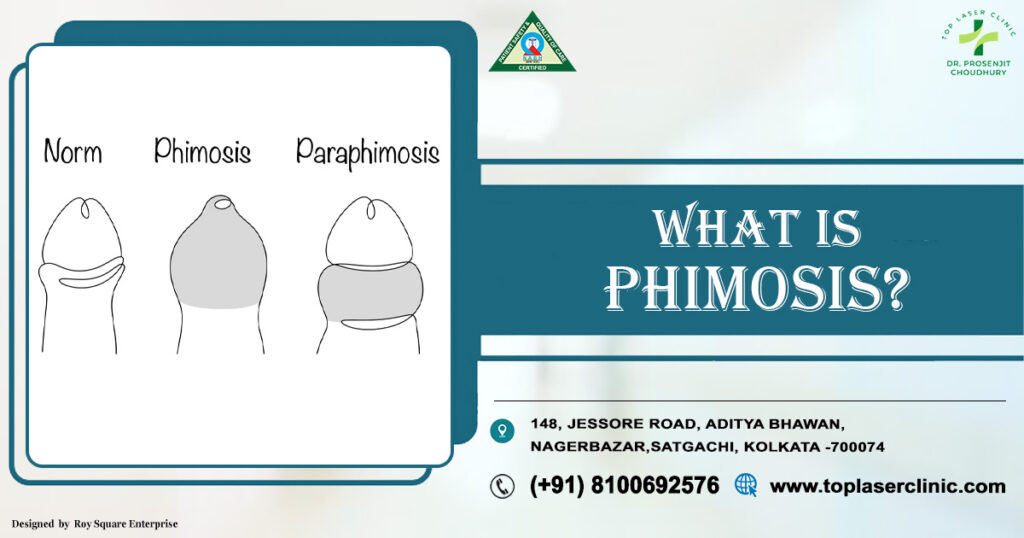
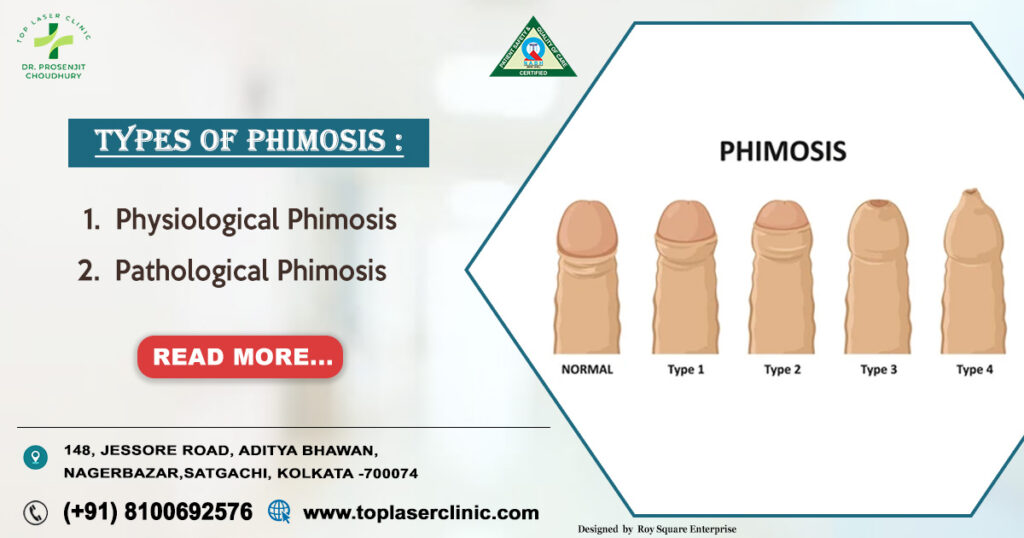
1. Phimosis (Tight Foreskin)
If you cannot retract your foreskin fully or it causes discomfort, pain, swelling, or infections, ZSR is highly suitable.
2. Paraphimosis
When the foreskin gets stuck behind the glans and cannot return to its normal position, ZSR circumcision can be a permanent solution.
3. Recurrent Foreskin Infections
Frequent balanitis, itching, redness, or foul smell makes you a good candidate for ZSR.
4. Frenulum Breve (Short Frenulum)
A short frenulum that causes tearing or pain during intercourse can be corrected with ZSR.
5. Pain or Discomfort during Intercourse
If your foreskin causes friction, tightness, cracks, or pain, ZSR helps improve sexual comfort.
6. Hygiene Difficulties
If maintaining foreskin hygiene is difficult, ZSR provides a long-term hygienic advantage.
7. Cosmetic Preference
Individuals who want a cleaner, smoother, and neater cosmetic appearance often prefer ZSR because it offers uniform, aesthetic results.
8. Medical Advice Based on Urology/Surgical Assessment
Sometimes doctors recommend ZSR to prevent future complications—especially if you have diabetes or are prone to infections.
Who Should Avoid ZSR?
You may not be the right candidate if:
- You have active genital infections
- You have bleeding disorders
- You have severe uncontrolled diabetes
- You have anatomical abnormalities requiring a different surgical approach
In such cases, the surgeon will decide the safest alternative.
Why Many Patients Prefer ZSR
- Very little pain
- Quick procedure (10–15 minutes)
- Faster healing
- Minimal bleeding
- Great cosmetic finish
- High satisfaction rate

Causes That Lead People to Choose ZSR
People opt for ZSR circumcision for several medical or personal reasons:
- Phimosis (tight foreskin that doesn’t retract)
- Paraphimosis (trapped retracted foreskin)
- Recurrent infections like balanitis
- Pain during intercourse due to tight foreskin
- Poor hygiene leading to repeated irritation
- Cultural or religious preferences
- Cosmetic enhancement
- Improved sexual comfort
ZSR becomes the ideal choice when someone wants an effective solution with the least pain and downtime.
Risk Factors That May Indicate You Are an Ideal Candidate
Certain conditions make ZSR circumcision highly beneficial:
- a. Chronic foreskin infections
- b. Poor retractability
- c. Frequent UTIs
- d. Painful erections due to tight foreskin
- e. Diabetes (higher infection risk with traditional surgeries)
- f. Sensitive penile skin
- g. Desire for quick recovery
- h. Fear of major bleeding or open surgery
- i. Busy lifestyle with less downtime
At Top Laser Clinic, Dr. Prosenjit Choudhury evaluates each patient individually to confirm whether ZSR is the safest and most effective option.
Diagnosis: How Doctors Assess If You’re the Right Candidate
To determine whether you are an ideal candidate for ZSR circumcision, the doctor will:
- Perform a physical examination
- Review medical history
- Check for infections
- Assess foreskin condition
- Evaluate retractability
- Identify any underlying health conditions
- Perform lab tests if required (especially for diabetics)
This ensures that patients receive the safest treatment plan tailored to their condition.
Dr. Prosenjit Choudhury, an experienced General & Laparoscopic Surgeon in Kolkata, uses a thorough diagnostic approach to ensure each patient is perfectly suited for the ZSR method.
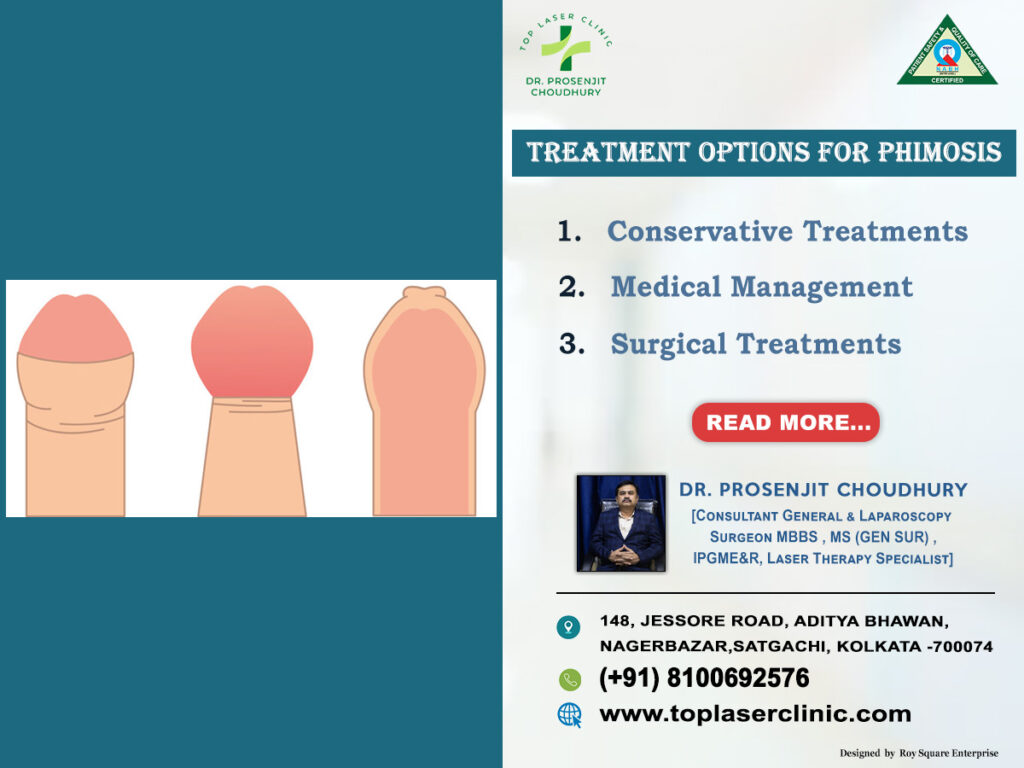
Treatment Options for Foreskin Problems (Including ZSR)
While ZSR is highly preferred, doctors consider all treatment options before recommending circumcision.
A. Medical Treatments
- Antibiotics for infections
- Ointments or creams for mild phimosis
- Steroid creams
These work only in mild cases.
B. Traditional Circumcision
More invasive, longer healing time, and more visible stitches.
C. Laser Circumcision
Better than traditional, but still more downtime compared to ZSR.
D. ZSR Stapler Circumcision
The most advanced option with benefits like:
- Minimal bleeding
- Almost painless
- Stitch less
- Highly aesthetic finish
- Quick procedure
- Fast recovery
This is why stapler circumcision is the preferred treatment for many patients dealing with foreskin issues.
Recovery After stapler circumcision Circumcision
One of the biggest reasons patients choose stapler circumcision is the smooth recovery.
Typical Recovery Timeline:
Day 1–3:
Mild discomfort or swelling. Normal.
Day 4–7:
Most swelling reduces. Staples begin loosening naturally.
Day 10–14:
Staples fall off on their own.
Within 2 weeks:
Most patients return to normal activities.
Within 4–6 weeks:
Complete healing, including sexual activity.
Recovery Tips:
- Keep the area clean and dry
- Wear loose clothing
- Avoid strenuous exercise for 1–2 weeks
- Follow medication instructions
- Maintain hygiene
- Attend follow-up visits
Under Dr. Prosenjit Choudhury at Top Laser Clinic, patients receive clear post-care instructions to ensure a smooth recovery process.
Complications: Are There Any?
stapler circumcision circumcision is considered very safe, but like any medical procedure, minor complications may occur:
- Mild temporary swelling
- Slight bleeding
- Discomfort for a few days
- Rarely, infection (preventable with proper care)
- Allergic reaction to anaesthesia (very rare)
The overall complication rate is extremely low, especially when performed by an experienced specialist.
Top 10 FAQs About Stapler Circumcision
1. Is stapler circumcision painful?
Most patients feel only mild discomfort. It’s far less painful than traditional surgery.
2. How long does the stapler circumcision procedure take?
Usually 10–20 minutes.
3. Is it safe for adults?
Yes, it’s one of the safest and most recommended techniques for adults.
4. Will there be visible stitches?
No. The stapler seals the wound automatically.
5. When can I resume work?
Most people return to work in 2–3 days.
6. When can I have sex again?
Usually after 4–6 weeks, once fully healed.
7. Will it improve hygiene?
Yes, circumcision reduces infections and improves overall hygiene.
8. Can diabetics undergo stapler circumcision?
Yes. It’s safer for diabetics because it reduces infection risk.
9. Are the results permanent?
Yes, the foreskin is permanently removed.
10. Who performs stapler circumcision?
It is performed by trained surgeons. At Top Laser Clinic, Dr. Prosenjit Choudhury specializes in stapler circumcision and modern circumcision procedures.
Why Choose Dr. Prosenjit Choudhury, Top Laser Clinic
When choosing a circumcision method, the surgeon’s expertise matters as much as the technique.
Here’s why patients trust Dr. Prosenjit Choudhury:
- Highly experienced General & Laparoscopic Surgeon in Kolkata
- Expert in stapler circumcision, laser, and minimally invasive procedures
- Uses advanced tools and technology
- Ensures painless, safe, and quick procedures
- Provides personalized treatment plans
- Maintains excellent hygiene and safety protocols
- Offers comfortable recovery support
If you’re searching for the best general surgeon in Kolkata, Dr. Prosenjit Choudhury at Top Laser Clinic is one of the most reliable and highly recommended names for stapler circumcision circumcision.
Conclusion
stapler circumcision circumcision has transformed the way circumcision is performed today. With its modern technology, minimal discomfort, quick recovery, and clean cosmetic results, it has become the first choice for many individuals dealing with foreskin-related issues.
The ideal candidate for stapler circumcision is someone who wants a safe, fast, hygienic, and comfortable circumcision experience—without the complications of traditional surgery.
Whether you’re dealing with phimosis, infections, pain, or simply want a modern and effective option, stapler circumcision is an excellent solution.
For expert guidance, safe treatment, and a reassuring experience, Dr. Prosenjit Choudhury at Top Laser Clinic offers comprehensive care backed by years of surgical expertise.