Breast health is one of the most important aspects of a woman’s well-being. Detecting the early signs of a breast tumour can save lives through timely diagnosis and treatment. With advancements in modern healthcare, awareness and regular check-ups have become key to prevention and early detection.
At Top Laser Clinic, Kolkata, under the expert care of Dr. Prosenjit Choudhury, Consultant General & Laparoscopy Surgeon, MBBS, MS (Gen Sur.), IPGME&R, Best in Laser & Minimally Invasive Surgery, patients receive top-quality care using advanced diagnostic and surgical methods. Recognized as the best general surgeon in Kolkata, Dr. Choudhury specializes in precise and minimally invasive treatments for various surgical conditions, including breast tumours.
What Is a Breast Tumour?
A breast tumour refers to an abnormal growth of cells within the breast tissue. These cells can be benign (non-cancerous) or malignant (cancerous). Early detection is crucial because malignant tumours can spread to other parts of the body if not treated promptly.
Breast tumours can develop in both men and women, though they are far more common in women.
Early Symptoms of a Breast Tumour
Recognizing symptoms early makes treatment much easier and more effective. Common signs include:
- A new lump or thickened area in the breast or underarm
- Change in breast size or shape
- Unexplained pain in the breast or nipple area
- Redness, swelling, or irritation on the skin
- Dimpling or puckering of the breast skin
- Fluid or blood-stained discharge from the nipple
- Inverted or retracted nipple
- Unusual hardness or heaviness in one breast
- Persistent itching around the nipple area
- Visible veins or changes in skin colour
If you notice any of these, consult Dr. Prosenjit Choudhury, the best general surgeon in Kolkata, for a proper examination and diagnosis at Top Laser Clinic, Kolkata.

Types of Breast Tumours
Breast tumours are generally classified as:
- Benign Tumours (Non-Cancerous):
- Fibroadenoma – Smooth, movable, non-cancerous lumps
- Cysts – Fluid-filled sacs that are harmless but may cause discomfort
- Malignant Tumours (Cancerous):
- Invasive Ductal Carcinoma (IDC) – Most common type
- Invasive Lobular Carcinoma (ILC) – Begins in the lobules
- Inflammatory Breast Cancer – Rare but aggressive form
Causes of Breast Tumours
The exact cause isn’t always clear, but several factors contribute to abnormal breast cell growth:
- Genetic mutations (like BRCA1 and BRCA2 genes)
- Hormonal imbalance (especially estrogen)
- Family history of breast cancer
- Long-term exposure to radiation
- Sedentary lifestyle and poor diet
- Obesity or being overweight
- Early menstruation or late menopause
Risk Factors
Some people are at higher risk of developing breast tumours due to:
- Age: Risk increases after 40
- Gender: Women are more prone than men
- Genetics: Inherited mutations in certain genes
- Hormonal Therapy: Long-term use of hormone-based medications
- Lifestyle Choices: Smoking, alcohol, and unhealthy eating
- Lack of Physical Activity: Increases estrogen levels
- Stress and Sleep Deprivation
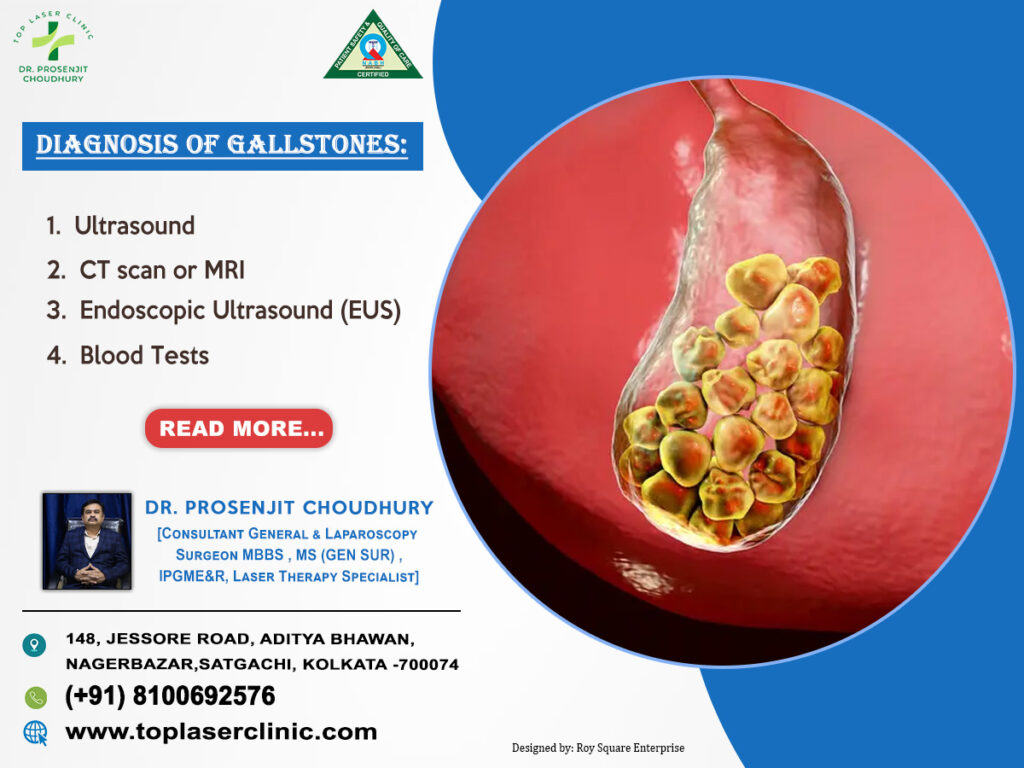
Diagnosis of Breast Tumour
Timely diagnosis plays a vital role in successful treatment. Dr. Prosenjit Choudhury at Top Laser Clinic, Kolkata uses a combination of modern diagnostic tools, including:
- Clinical Breast Examination (CBE) – Manual checking for lumps or changes
- Mammogram – X-ray imaging to detect lumps before they are felt
- Ultrasound – Distinguishes between solid and fluid-filled lumps
- MRI Scan – Provides detailed images of breast tissues
- Biopsy – Confirms if a lump is benign or malignant
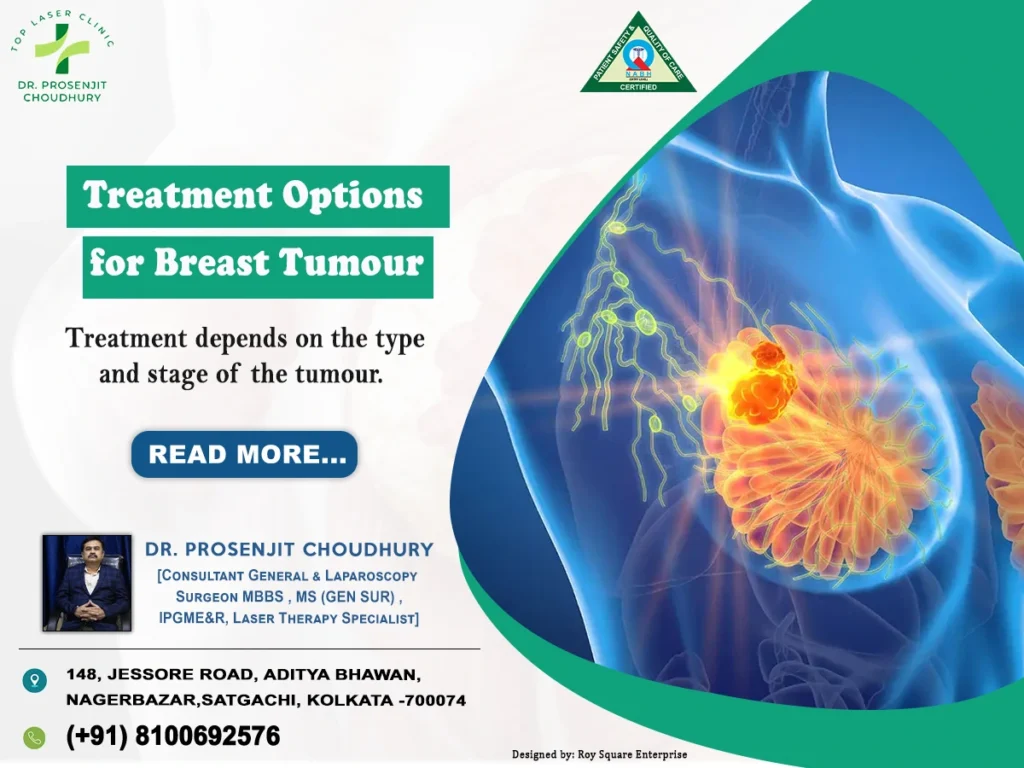
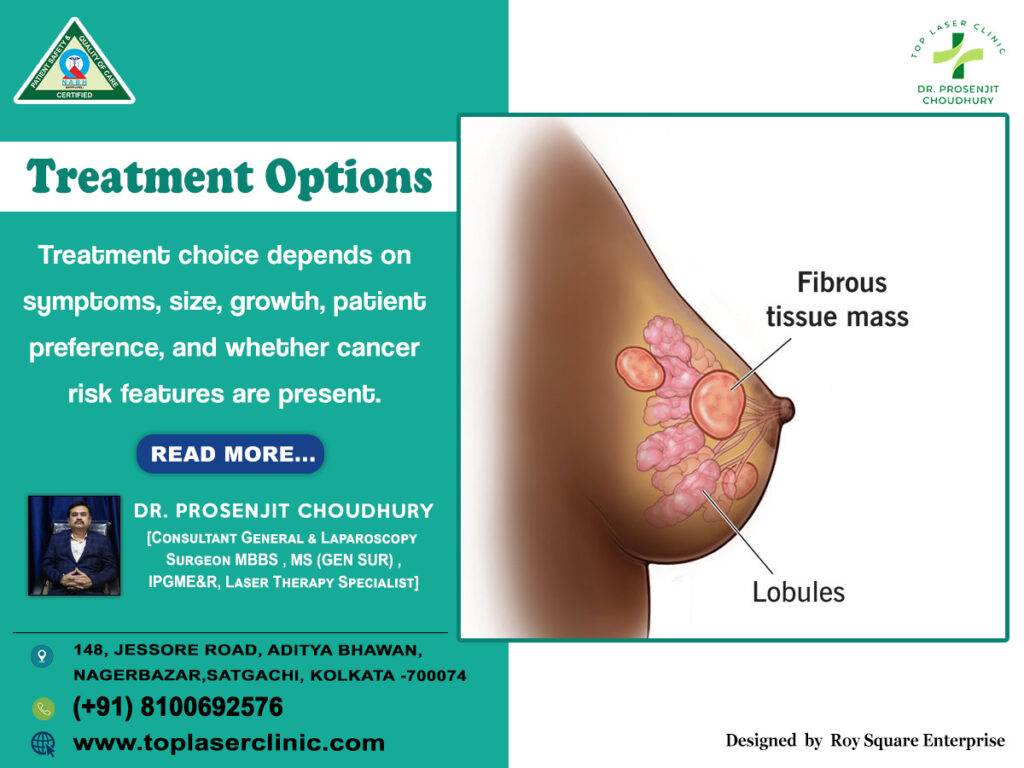
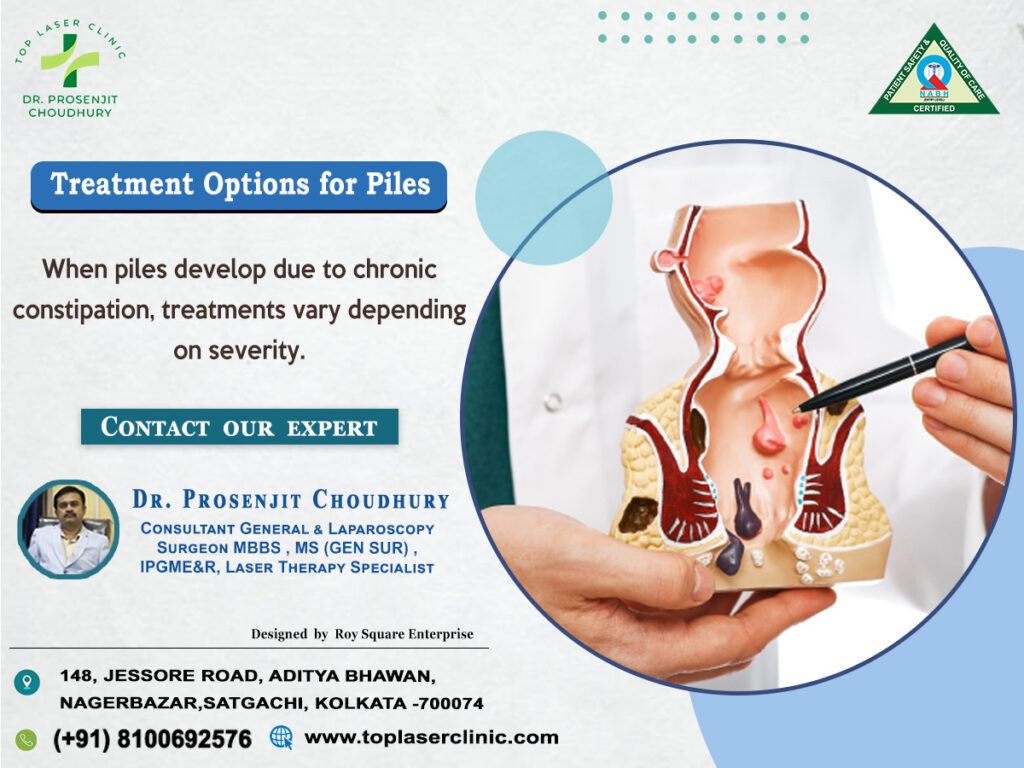
Treatment Options for Breast Tumour
Treatment depends on the type and stage of the tumour. Common approaches include:
- Medication & Hormone Therapy – For hormone-sensitive tumours
- Surgery
- Lumpectomy – Removes the lump and surrounding tissue
- Mastectomy – Removes one or both breasts in advanced cases
- Laparoscopic Surgery – Minimally invasive surgery with faster recovery
- Radiation Therapy – Kills remaining cancer cells after surgery
- Chemotherapy – Destroys rapidly growing cancer cells
- Targeted Therapy – Focuses on specific cancer cell genes and proteins
At Top Laser Clinic, Dr. Prosenjit Choudhury uses advanced laparoscopic and laser-assisted surgical methods, ensuring less pain, minimal scarring, and quicker recovery.
Recovery after Treatment
Recovery depends on the treatment type and patient’s overall health:
- Hospital Stay: 1–3 days for laparoscopic procedures
- Pain & Discomfort: Usually mild and controlled with medication
- Return to Routine: Within 2–3 weeks
- Follow-ups: Regular check-ups to monitor healing and detect recurrence
Proper guidance from Dr. Prosenjit Choudhury helps patients recover faster and maintain long-term wellness.
Possible Complications
Though most cases heal well with proper care, some potential complications may include:
- Infection at the surgical site
- Swelling or fluid accumulation
- Scarring or numbness
- Emotional distress or anxiety
- Risk of recurrence (in malignant cases)
Close medical supervision at Top Laser Clinic, Kolkata minimizes such risks effectively.
Top 10 FAQs about Breast Tumour
- Is every breast lump cancerous?
No, most lumps are benign, but they should always be examined by a doctor. - Who is most at risk?
Women over 40 and those with a family history are at higher risk. - Can men develop breast tumours?
Yes, although rare, men can also have breast tumours. - Is breast pain always a sign of cancer?
Not necessarily. Hormonal changes or infections can also cause pain. - Can lifestyle changes reduce my risk?
Yes, a balanced diet, regular exercise, and limiting alcohol can help. - How often should I get screened?
Women over 40 should get a mammogram every 1–2 years. - Can breast cancer be cured if detected early?
Yes, early-stage detection has a high success and survival rate. - What is the role of laparoscopic surgery in breast tumour treatment?
It offers precise removal with less pain, smaller scars, and faster healing. - Are there side effects of breast tumour treatment?
Some patients may experience fatigue, nausea, or mild discomfort post-treatment. - Who is the best surgeon for breast tumour treatment in Kolkata?
Dr. Prosenjit Choudhury, at Top Laser Clinic, Kolkata, is highly trusted for his expertise in laser and minimally invasive surgeries.
Why Choose Top Laser Clinic, Kolkata?
- Experienced Surgeon: Dr. Prosenjit Choudhury, MBBS, MS (Gen Surg), IPGME&R — one of Kolkata’s most respected laparoscopic and general surgeons.
- Advanced Technology: State-of-the-art laser and laparoscopic equipment for precise diagnosis and treatment.
- Comprehensive Care: From screening to recovery, every step is carefully guided.
- Patient Safety First: Focused on pain-free, minimally invasive procedures.
- Affordable Excellence: Quality healthcare at reasonable costs.
Conclusion
Recognizing the early signs of breast tumour can make a life-saving difference. Regular self-examinations, awareness, and timely medical consultation are vital. With modern treatment methods like laparoscopic and laser-assisted surgeries, patients now have access to faster healing, minimal pain, and better results.
At Top Laser Clinic, Kolkata, Dr. Prosenjit Choudhury, the best general surgeon in Kolkata, leads the way in offering expert care and advanced treatments. His patient-focused approach and vast surgical experience ensure the best possible outcomes for those battling breast health concerns.
If you or a loved one notices any unusual changes in your breast, don’t wait. Visit Top Laser Clinic and consult Dr. Prosenjit Choudhury for a thorough evaluation and personalized treatment. Early diagnosis saves lives — takes the first step today toward better health.