Introduction
Phimosis, also known as Tight foreskin is a condition that affects males of different age groups and is often surrounded by stigma, misconceptions, and hesitation to seek medical help. It is a medical condition in which the foreskin of the penis cannot be retracted completely over the glans. While it can be normal in infants and young children, persistent phimosis in adults may cause discomfort, infections, and even complications if left untreated.
According to Dr Prosenjit Choudhury, Consultant General & Laparoscopy Surgeon | MBBS, MS (Gen Surg.), IPGME&R | Best in Laser & Minimally Invasive Surgery, at Top Laser Clinic timely diagnosis and the right treatment plan can effectively resolve phimosis without affecting one’s overall health or masculinity. Unfortunately, lack of awareness and myths prevent many individuals from getting medical consultation.
In this comprehensive guide, we will cover the description, symptoms, types, causes, treatment, myths vs. facts, and frequently asked questions about phimosis, while emphasizing the importance of seeking professional medical advice from experienced specialists.
What is Phimosis?
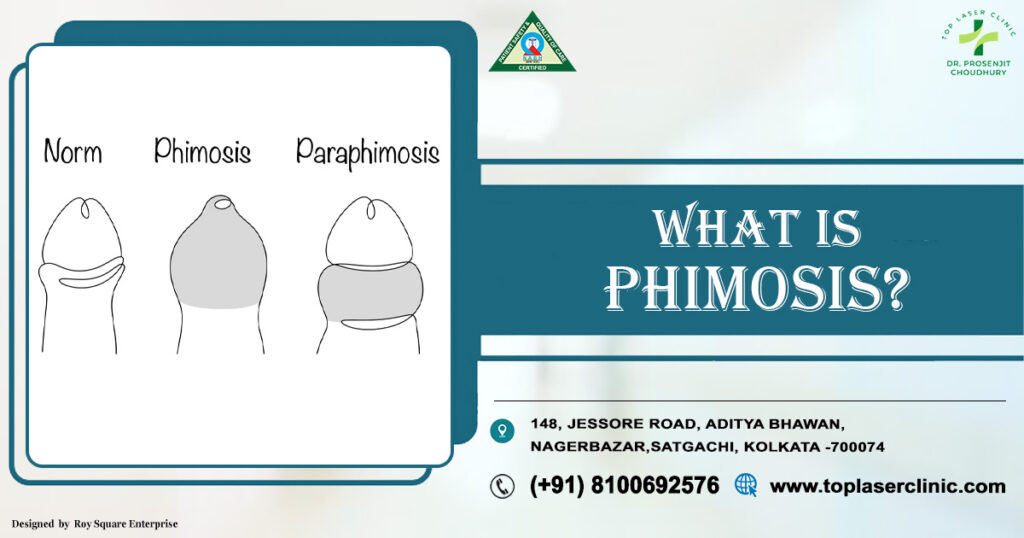
Phimosis is a condition where the foreskin (prepuce) is too tight to be pulled back over the head (glans) of the penis. It is commonly seen in infants and young boys as part of natural development, but in some cases, it may persist into adolescence or adulthood.
Phimosis itself is not always harmful. In many cases, it resolves naturally. However, pathological phimosis, which develops due to scarring, infections, or underlying conditions, requires medical intervention.
Symptoms of Phimosis
Symptoms of phimosis vary depending on severity and underlying causes. Common symptoms include:
- Tight foreskin that cannot be retracted.
- Swelling of the foreskin during urination.
- Pain or discomfort during sexual activity.
- Difficulty maintaining hygiene due to inability to clean under the foreskin.
- Recurrent infections (banalities or urinary tract infections).
- Ballooning of foreskin while passing urine.
- Redness, soreness, or cracks in the foreskin.
If these symptoms persist, it is essential to consult a surgeon or urologist to avoid long-term complications.
Types of Phimosis
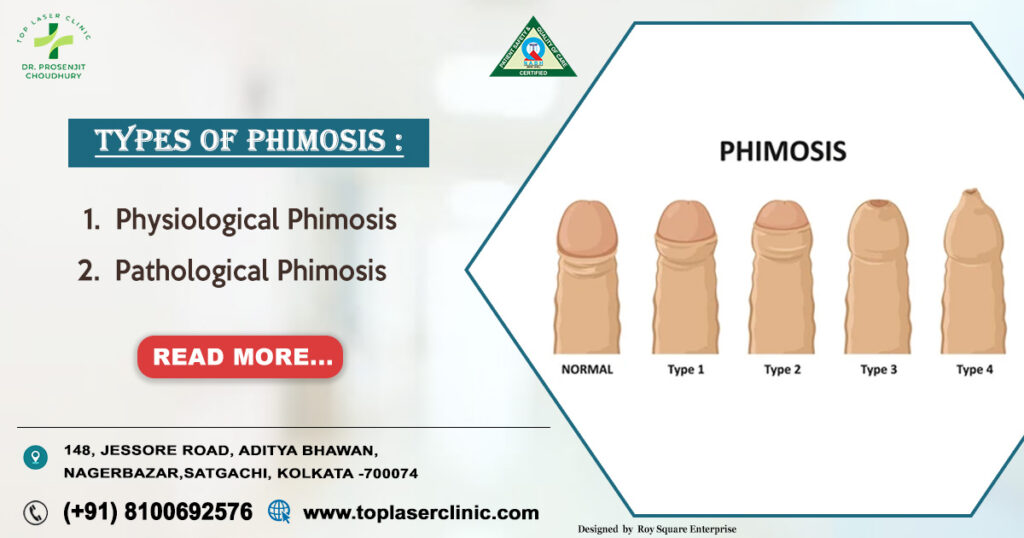
Phimosis can be classified into two main categories:
1. Physiological Phimosis
- Naturally present in infants and children.
- Usually resolves by adolescence.
- No treatment required unless it causes repeated infections or urinary issues.
2. Pathological Phimosis
- Occurs due to scarring, trauma, or chronic infection.
- Commonly seen in adults.
- Requires medical or surgical treatment.
Dr. Prosenjit Choudhury emphasizes that distinguishing between physiological and pathological phimosis is critical before deciding on treatment.
Causes of Phimosis
Several factors can lead to pathological phimosis:
- Poor hygiene leading to infections.
- Chronic balanitis (inflammation of glans and foreskin).
- Recurrent urinary tract infections.
- Scarring due to forceful retraction of foreskin.
- Diabetes mellitus, which increases risk of infection.
- Lichen sclerosis (skin condition causing white patches and scarring).
- Injury or trauma to foreskin.
As highlighted above, maintaining genital hygiene and avoiding forceful retraction during childhood are vital preventive steps.
Diagnosis of Phimosis
A specialist Sureon usually diagnoses phimosis through:
- Physical examination of the foreskin and glans.
- Patient history (symptoms, infections, trauma, medical conditions).
- Lab tests (urine analysis, blood sugar levels) if infections or diabetes are suspected.
Treatment Options for Phimosis or Tight Foreskin
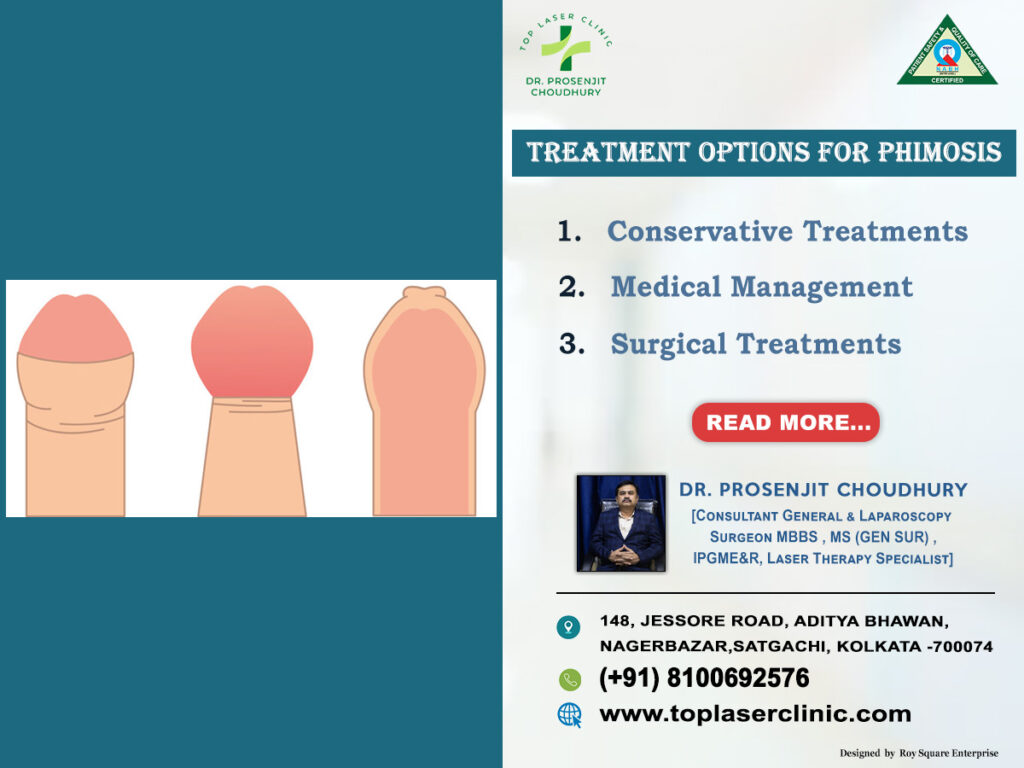
Treatment depends on the severity, age, and overall health of the patient. Dr. Prosenjit Choudhury recommends tailored treatment approaches for each patient.
1. Conservative Treatments
- Topical steroid creams: Help soften foreskin and reduce inflammation.
- Gentle stretching exercises: Under medical supervision, to widen foreskin opening.
- Improved hygiene practices.
2. Medical Management
- Antibiotics/antifungal medication for underlying infections.
- Anti-inflammatory treatment for skin conditions.
3. Surgical Treatments
- Circumcision: Complete removal of foreskin; permanent cure for Tight foreskin.
- Preputioplasty: A foreskin-preserving surgery that widens the opening.
- Dorsal slit procedure: Partial relief for tight foreskin without full removal.
According to Dr. Prosenjit Choudhury, minimally invasive surgical techniques such as laser circumcision are highly effective and ensure faster recovery with minimal pain.
Complications of Untreated Phimosis
If Tight foreskin is left untreated, it may lead to:
- Recurrent urinary tract infections.
- Painful erections and sexual dysfunction.
- Increased risk of paraphimosis (trapped foreskin).
- Higher chances of penile cancer (rare but documented).
- Chronic balanitis or skin scarring.
Final Thoughts
Tight foreskin is a manageable condition that should not be ignored or stigmatized. With proper awareness, timely consultation, and effective treatment, patients can live a healthy and confident life. Dr. Prosenjit Choudhury, stresses the importance of early medical intervention for better outcomes.
By understanding the myths, symptoms, and available treatments, individuals can make informed choices and avoid complications. If you or a loved one is experiencing symptoms of Tight foreskin, do not hesitate to seek expert medical advice.
Top 10 Frequently Asked Questions (FAQs)
1. Is Tight foreskin common?
Yes, it is common in children but often resolves naturally. Persistent adult Tight foreskinrequires medical attention.
2. Does Tight foreskin always need surgery?
No, as Dr. Prosenjit Choudhury highlights, many cases can be treated with creams and stretching exercises. Surgery is only needed in severe cases.
Can Tight foreskin cause infertility?
Not directly, but if untreated, it may cause infections and painful intercourse, indirectly affecting fertility.
4. Is circumcision the best solution?
Circumcision is a permanent cure, but alternative options exist. The best treatment depends on individual cases.
5. Can diabetes worsen Tight foreskin?
Yes, uncontrolled diabetes increases risk of infection and scarring, worsening Tight foreskin.
6. How long is recovery after surgery?
With advanced techniques used by surgeons, recovery is usually within 7–10 days.
7. Can Tight foreskin come back after treatment?
If proper care is taken, recurrence is rare. Preputioplasty may carry a slightly higher recurrence risk compared to circumcision.
8. Can Tight foreskin be treated at home?
Mild cases may improve with hygiene and prescribed creams, but home remedies alone are not sufficient.
9. Is Tight foreskin linked to cancer?
Untreated Tight foreskin increases the risk of penile cancer, though the overall risk is low.
10. When should I consult a doctor?
If you experience pain, infections, difficulty urinating, or sexual discomfort, consult specialists like Dr. Prosenjit Ch