Table of Contents
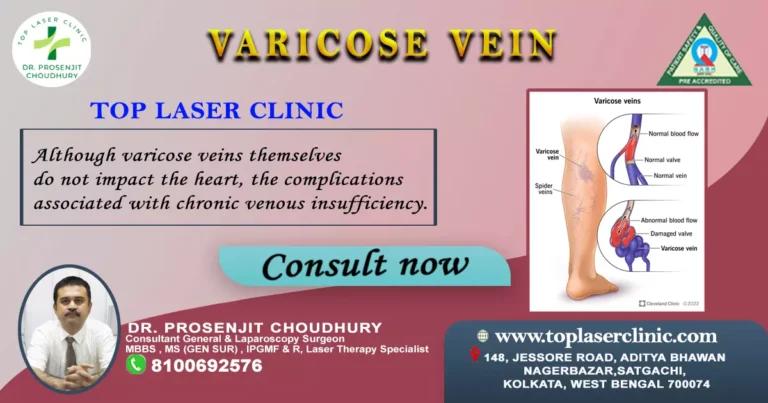
Varicose veins are a common condition that affects many individuals, causing discomfort and aesthetic concerns. Fortunately, there are various treatment options available to alleviate the symptoms and improve the appearance of varicose veins.One alternative treatment that has gained popularity recently is the use of mudras for varicose veins relief.
Mudras, which are hand gestures or positions, have been a part of traditional Indian and yogic practices for centuries. These mudras are believed to stimulate energy flow and promote healing in the body.
While there is no specific “mudra” (hand gesture) that directly targets varicose veins, some mudras and yoga practices may help improve circulation and promote overall well-being, which could indirectly benefit varicose veins.
Varicose veins are primarily a medical condition, and it’s important to consult with a healthcare professional for proper diagnosis and treatment.
However, here’s 3 Mudras for Varicose Vein that you could try, which may help promote circulation and alleviate discomfort associated with varicose veins:

1. Apana Mudra:
The Apana Mudra is believed to have various benefits, including improving circulation and aiding in detoxification. While there is no direct scientific evidence that Apana Mudra specifically targets varicose veins, it may contribute to overall well-being and potentially support better circulation. It’s important to note that mudras and holistic practices are not a replacement for medical treatment.
Here’s how to perform the Apana Mudra:
- Sit comfortably in a quiet and peaceful place.
- Keep your back straight and your hands resting on your thighs.
- Gently touch the tips of your middle finger and ring finger to your thumb, while extending your index finger and little finger.
- Relax your hands and arms.
- Close your eyes and take slow, deep breaths. You can also focus on your breath or a positive intention while holding the mudra.
- Hold the mudra for about 15-30 minutes.
2. Legs-Up-the-Wall Pose (Viparita Karani):
Legs-Up-the-Wall Pose (Viparita Karani) is a yoga posture that may help improve circulation and reduce swelling in the legs. While it’s not a direct treatment for varicose veins, it can be a beneficial practice to incorporate into your routine to support overall leg health. As always, consult with a healthcare professional before starting any new exercise or yoga practice, especially if you have a medical condition like varicose veins.
To practice Legs-Up-the-Wall Pose:
- Locate a spot against a clear wall where you can lie down comfortably with your legs extended vertically up the wall.
- Sit sideways against the wall, with your hips touching the wall and your knees bent.
- As you lie down, gently swing your legs up along the wall, so your body forms an “L” shape.
- You can adjust your distance from the wall to find a comfortable stretch. Your hips should be supported by the wall, and your legs should be straight up.
- Relax your arms by your sides, palms facing up.
- Close your eyes and take slow, deep breaths. Relax into the pose, allowing your muscles to release tension.
- Stay in this pose for 5 to 15 minutes, or as long as you feel comfortable. Try to relax and pay attention to your breath.
- To come out of the pose, gently bend your knees and roll onto one side. Take a moment before slowly sitting up.
Legs-Up-the-Wall Pose can help with relaxation, circulation, and reducing pressure in the legs. It’s also a great way to relieve stress and promote a sense of calm. However, it’s important to remember that this pose may not be suitable for everyone, especially if you have certain medical conditions. Always prioritize your safety and consult with a healthcare professional if you have any concerns about practicing yoga poses, especially if you’re dealing with varicose veins.

3. Gyan Mudra:
The Gyan Mudra is a popular hand gesture used in yoga and meditation. It is believed to have various mental and spiritual benefits.
To perform the Gyan Mudra:
- Sit in a comfortable meditation posture, such as Padmasana (Lotus Pose), Sukhasana (Easy Pose), or any other comfortable seated position.
- Keep your spine straight and your hands resting on your knees or thighs.
- Touch the tip of your thumb to the tip of your index finger (also known as the Jupiter finger).
- The other three fingers (middle, ring, and little fingers) should remain extended or slightly relaxed.
The Gyan Mudra is thought to represent knowledge, wisdom, and the connection between individual consciousness and universal consciousness.
It is believed that practicing this mudra can help enhance concentration, memory, and mental clarity. It is often used during meditation or pranayama (breath control) practices to facilitate a calm and focused mind.
In closing:
Remember that these practices are not a substitute for medical treatment. If you have varicose veins or any other medical condition, it’s important to consult a healthcare professional before trying any new practices. They can provide you with appropriate guidance and recommendations based on your individual health needs.