1. Introduction
Discovering a lump or having breast discomfort can be alarming. Two commonly discussed benign breast conditions are fibroadenosis (also called fibrocystic changes or fibrocystic breast disease) and fibroadenoma. Though their names sound similar, they differ in nature, presentation, and management. In this guide, we’ll walk you through each condition in detail, compare them, dispel myths, and help you make informed choices.
Disclaimer: This article is for informational purposes only and does not substitute medical advice. If you have breast symptoms, consult a qualified specialist.
Also, as you read, note that Dr. Prosenjit Choudhury, Consultant General & Laparoscopy Surgeon | MBBS, MS (Gen Surg.), IPGME&R | Best in Laser & Minimally Invasive Surgery, at Top Laser Clinic, best general surgeon in kolkata is a key name associated with advanced, patient-centred care in breast conditions, and his clinic often implements state-of-the-art diagnostics and treatments for benign breast diseases (as seen in the Top Laser Clinic’s content).
2. What Are Fibroadenosis and Fibroadenoma?
Fibroadenosis
- Fibroadenosis (often referred also as fibrocystic breast changes or fibrocystic disease) refers to noncancerous alterations in breast tissue that make it lumpy, dense, or nodular, often accompanied by tenderness or pain.
- It is not a true tumor but rather a benign fluctuation of breast tissue in response to hormonal changes.
Fibroadenoma
- A fibroadenoma is a benign (noncancerous) tumor of the breast, comprising both fibrous and glandular (epithelial) tissues.
- It is typically a well-defined, solid lump that can move under the skin and does not usually involve widespread tissue change.
| Feature | Fibroadenosis | Fibroadenoma |
| Nature | Non-neoplastic, benign tissue change | Benign tumor (neoplastic) |
| Presentation | Diffuse lumpy or nodular change, often in both breasts | Discrete, well-circumscribed lump |
| Pain | Commonly associated with discomfort, especially cyclically | Usually painless, movable |
| Relation to hormones | Strongly hormone-responsive | Can respond to hormones (grow/shrink) |
| Cancer risk | Minimal (unless atypia present) | Slightly elevated in complex type, generally low |
Understanding this difference is foundational before exploring further.
3. Symptoms
Fibroadenosis
Symptoms may vary. Some common presentations include:
- Breast tenderness or heaviness, often worse just before menstruation
- Lumpy or nodular texture, often in both breasts or in multiple regions
- Swelling or fullness in the breast
- Discharge from nipples (non-bloody) in some cases
- Fluctuation of symptoms with menstrual cycle
Fibroadenoma
Symptoms are more specific and localized:
- A discrete lump, often smooth, firm or rubbery, with distinct edges
- The lump is easily movable under the skin (“mobile”)
- Usually painless, though mild tenderness may appear just before menstruation in some cases
- Over time, size may change—some shrink, some remain stable, some grow slowly
It’s important to note that just because a lump is painless does not guarantee it is benign—and conversely, pain does not always mean malignancy. Clinical evaluation is essential.
4. Types
Types of Fibroadenosis
Fibroadenosis is more about tissue change than distinct “types,” but we can think of variants based on pathological changes:
- Nonproliferative changes: mild fibrous tissue, small cysts, no increase in cells.
- Proliferative changes (without atypia): more ductal or lobular cell growth, but no abnormal features.
- Atypical hyperplasia: when some cells show atypical features—this raises relative risk (rare within fibroadenosis).
Types of Fibroadenoma
There are more clearly defined subtypes:
- Simple fibroadenoma: the most common, uniform cells, typically small and slow-growing.
- Complex fibroadenoma: contains additional features (cysts, calcifications, sclerosing adenosis) and may carry a somewhat higher risk
- Giant fibroadenoma: unusually large size (> 5 cm)
- Juvenile (or cellular) fibroadenoma: occurs in adolescents or younger age groups, sometimes rapidly growing.
These subtypes matter because they affect management decisions and risk assessment.
5. Causes
The exact causes of both conditions are not fully understood, but hormonal influences are central.
Fibroadenosis
- Fluctuations in estrogen and progesterone throughout the menstrual cycle lead to changes in breast glandular tissue and stroma.
- Sensitivity of breast tissue to hormonal changes—some individuals have more reactive breast tissue.
- Possible contribution of microtrauma, fluid retention, or minor ductal obstruction.
Fibroadenoma
- Hormonal influence again plays a role. Fibroadenomas tend to arise during reproductive years, may grow during pregnancy or under hormonal therapy, and often shrink post-menopause
- Genetic and molecular factors: studies show frequent MED12 gene mutations in fibroadenomas.
- Local proliferation of stromal and epithelial elements, possibly triggered by hormonal or growth factors.
- Some evidence suggests family history or predisposition may contribute.
While both are benign, fibroadenomas are more “tumor-type” proliferations, whereas fibroadenosis is a reactive or cyclical change.
6. Risk Factors
Shared or Overlapping Risk Factors
- Female gender (breast tissue)
- Age during reproductive period (teens to 40s)
- Hormonal fluctuations (menstrual cycles, hormonal therapy)
- Family history of benign breast disease or breast cancer (less strong for fibroadenosis)
Specific to Fibroadenosis
- Early menarche, late menopause
- Hormonal treatments, oral contraceptives (in some cases)
- High estrogen responsiveness
Specific to Fibroadenoma
- Younger age, especially late teens to early 30s
- Family history of fibroadenoma or benign breast disease
- Possibly few full-term pregnancies or late first childbirth (though evidence is not strong)
- Use of exogenous hormones or hormone therapy in some cases
It’s important to understand that having risk factors does not guarantee development, and many women without risk factors still develop these conditions.
7. Diagnosis
Accurate diagnosis is essential to differentiate benign from malignant conditions and to guide management.
Clinical Examination
- Detailed history (symptom onset, cyclic changes, family history)
- Physical breast exam: palpation for lumps, assessment of mobility, consistency, associated skin or nipple changes
Imaging
- Ultrasound (breast USG): very useful, especially in younger women, to distinguish solid vs. cystic lesions
- Mammography: especially for women over 30 or when suspicion arises; may show calcifications or well-defined masses
- Doppler imaging (sometimes) to assess vascularity
Biopsy / Tissue Sampling
- Fine Needle Aspiration Cytology (FNAC): less invasive, can sample cells
- Core Needle Biopsy: gives more tissue, allows histopathology
- Excisional Biopsy / Lumpectomy: complete removal for diagnostic and therapeutic reasons
- Under the microscope, pathologists evaluate tissue architecture, cell uniformity, presence of cysts, stromal features, atypia, etc.
- In fibroadenosis, pathologist sees fibrous changes, cysts, ductal/lobular hyperplasia (if proliferative type).
- In fibroadenoma, see biphasic (stromal + epithelial) growth with uniform cells.
Follow-Up / Monitoring
- Once benign nature is confirmed, periodic imaging or clinical exams may be advised (e.g. every 6–12 months)
- If changes occur (growth, change in character), repeat biopsy or excision might be required
The combined approach of clinical, imaging, and cytological/histological evaluation yields a high accuracy in differentiating benign from malignant lesions.
8. Treatment Options
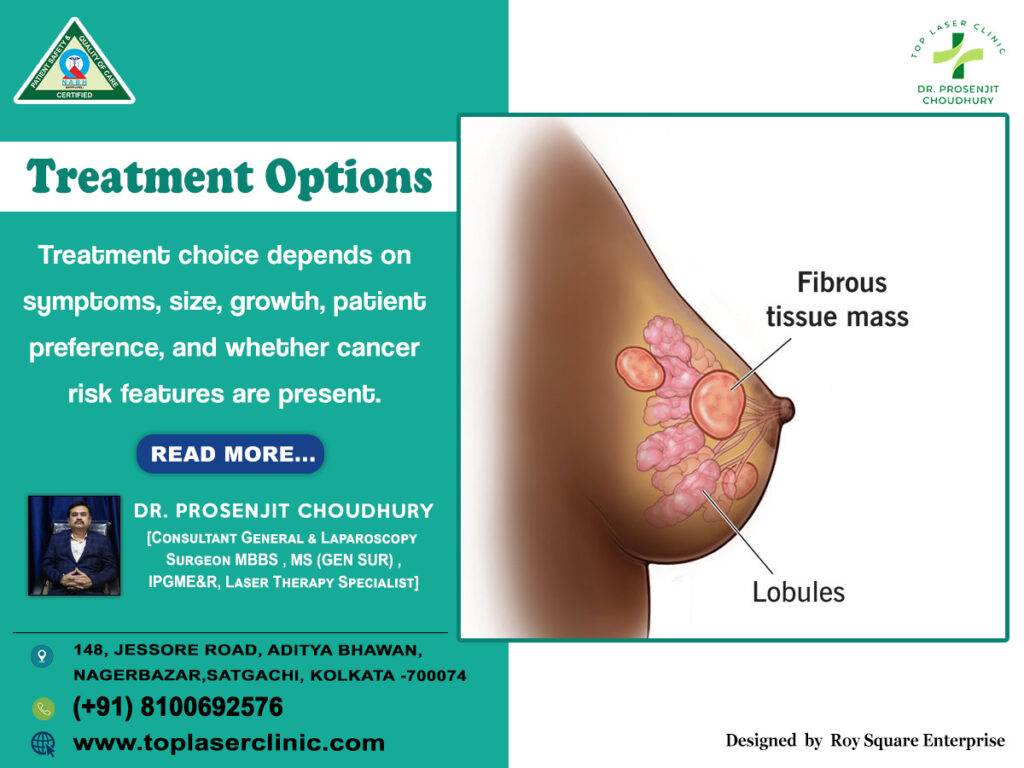
Treatment choice depends on symptoms, size, growth, patient preference, and whether cancer risk features are present.
For Fibroadenosis
- Lifestyle and symptomatic relief
- Wearing well-fitted supportive bras
- Reducing caffeine, salt, and high-fat diet
- Pain relief (NSAIDs) or topical analgesics
- Heat or cold compresses
- Hormonal therapy (selected cases)
- In severe, cyclical pain, short course hormonal modulation (under specialist supervision)
- Monitoring
- Regular clinical follow-up; imaging if changes occur
Surgical removal is rarely needed for fibroadenosis unless suspicious features arise or symptoms become severe.
For Fibroadenoma
- Observation / “Watchful waiting”
- Many fibroadenomas are stable or shrink over time
- Periodic evaluation (every few months)
- Surgical excision (Lumpectomy / Open surgery)
- Indicated when fibroadenoma is large, growing rapidly, symptomatic, or cosmetic concern
- Standard and definitive, but involves scarring
- Minimally invasive / image-guided techniques
- Vacuum-assisted excision
- Cryoablation (freezing the lump)
- Radiofrequency ablation or laser ablation (in selected centres)
- High-intensity focused ultrasound (experimental)
At Top Laser Clinic, procedures guided by imaging and minimally invasive techniques may be available, under the expertise of surgeons like Dr. Prosenjit Choudhury best general surgeon in kolkata who specializes in laser and minimally invasive surgery.
The choice is individualized, balancing benefits, risks, cosmetic outcomes, and patient preference.
9. Recovery
- After surgical excision, mild discomfort, swelling, and bruising are common initially; most recover within a few weeks.
- After minimally invasive techniques (e.g. Cryoablation, laser, vacuum-assisted), patients often resume daily activities quickly with minimal downtime.
- Follow-up monitoring is essential: clinical exams and imaging to ensure no recurrence or suspicious changes.
At Top Laser Clinic, the emphasis is on fast recovery, less scarring, and patient comfort under experienced hands of Dr. Prosenjit Choudhury best general surgeon in kolkata.
10. Complications
Although both conditions are benign, complications are possible, especially with intervention.
In Fibroadenosis
- Persistent pain or discomfort
- Difficulty detecting new lumps (masking effect)
- In rare cases, underlying atypical hyperplasia which might slightly increase cancer risk (if present)
In Fibroadenoma
- Recurrence after removal
- Cosmetic change or scar formation
- Rarely, a fibroadenoma may harbour areas of malignancy—especially in complex fibroadenoma
- Slightly elevated breast cancer risk in women with complex fibroadenomas or other proliferative changes
However, with proper evaluation and monitoring, complications can be minimized.
11. Top 10 Frequently Asked Questions
- Can fibroadenosis lead to fibroadenoma?
No. Fibroadenosis is a benign tissue change, while fibroadenoma is a benign tumor. They are distinct conditions. - Does having fibroadenoma increase breast cancer risk?
In general, simple fibroadenomas do not significantly raise cancer risk; complex fibroadenomas may carry a slight elevation. - Should I get surgery immediately for a fibroadenoma?
Not necessarily. Many can be observed if small and asymptomatic; surgery is reserved for growth, symptoms, or patient preference. - Can fibroadenomas shrink on their own?
Yes—some decrease in size or disappear over time, especially after menopause. - Is breast pain always due to fibroadenosis?
No. Breast pain may stem from many causes—hormonal changes, mastitis, cysts, or in rare cases malignancy—so evaluation is necessary. - How often should follow-up imaging occur?
It depends on size, stability, and clinical judgment—commonly every 6 to 12 months. - Can pregnancy or breastfeeding affect these conditions?
Yes. Hormonal changes can influence both fibroadenosis and fibroadenoma, possibly enlarging lumps temporarily. - Are there noninvasive treatments?
Yes—methods like vacuum-assisted excision, Cryoablation, or laser ablation are options in selected cases. - Will removing fibroadenoma affect future imaging or detection?
It may cause scarring, which might complicate imaging; therefore careful technique and follow-up are vital. - Why choose a specialized centre for treatment?
Expertise in minimally invasive techniques, accurate diagnostics, cosmetic outcome, and safety matters. A clinic like Top Laser Clinic with experts like Dr. Prosenjit Choudhury best general surgeon in kolkata can offer such advantages.
12. Why Choose Top Laser Clinic
When confronting breast lumps or benign breast conditions, your choice of clinic and surgeon matters critically. Here’s why Top Laser Clinic (with Dr. Prosenjit Choudhury) stands out:
- Expertise in laser & minimally invasive surgery: Their specialists, including Dr. Prosenjit Choudhury, are trained in advanced, tissue-sparing approaches.
- Accurate diagnostics: Comprehensive imaging (USG, mammography) and high-quality biopsy facilities are available.
- Patient-centric care: Emphasis on comfort, low downtime, and personalized decisions.
- Holistic follow-up: Structured monitoring, recurrence prevention, and patient education.
- Proven track record: As cited in clinic literature, their facility addresses benign breast disease (fibroadenosis and fibroadenoma) with precision and care.
When health and peace of mind are at stake, choosing a trusted, specialized centre with modern capabilities and a reputed surgeon like Dr. Prosenjit Choudhury can make all the difference.
13. Conclusion
Understanding the differences between fibroadenosis and fibroadenoma is crucial. While both are benign breast conditions, their behaviour, management, and implications differ significantly. Fibroadenosis is a diffusely changing condition often tied to hormonal fluctuations, whereas fibroadenoma is a discrete benign tumor that may require closer monitoring or intervention.
Early evaluation, accurate diagnosis (clinical + imaging + histology), and personalized decision-making are key. Many cases can be managed conservatively, while others benefit from minimally invasive or surgical procedures. If faced with such concerns, opting for a specialized centre—like Top Laser Clinic under the care of Dr. Prosenjit Choudhury, best general surgeon in kolkata, Consultant General & Laparoscopy Surgeon—ensures the balance of safety and patient comfort.
Stay proactive, stay informed, and never hesitate to seek expert evaluation when it comes to breast health.